Testicular Cancer
TESTİCULAR CANCER
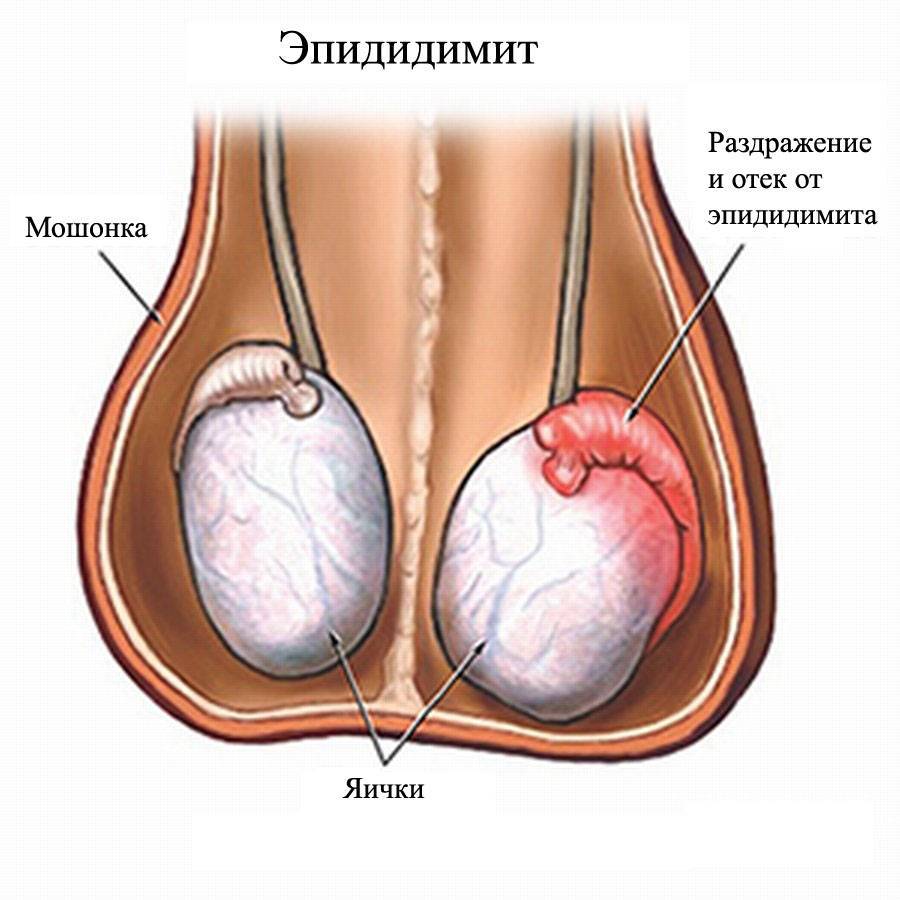
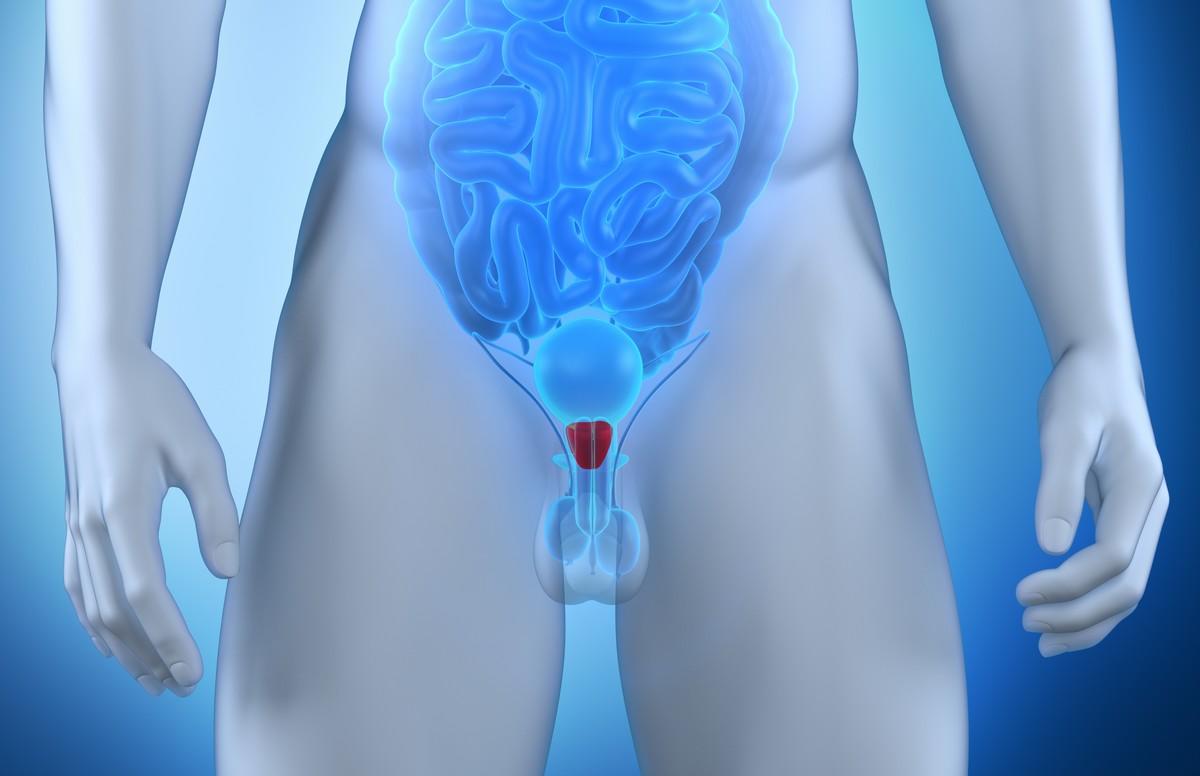
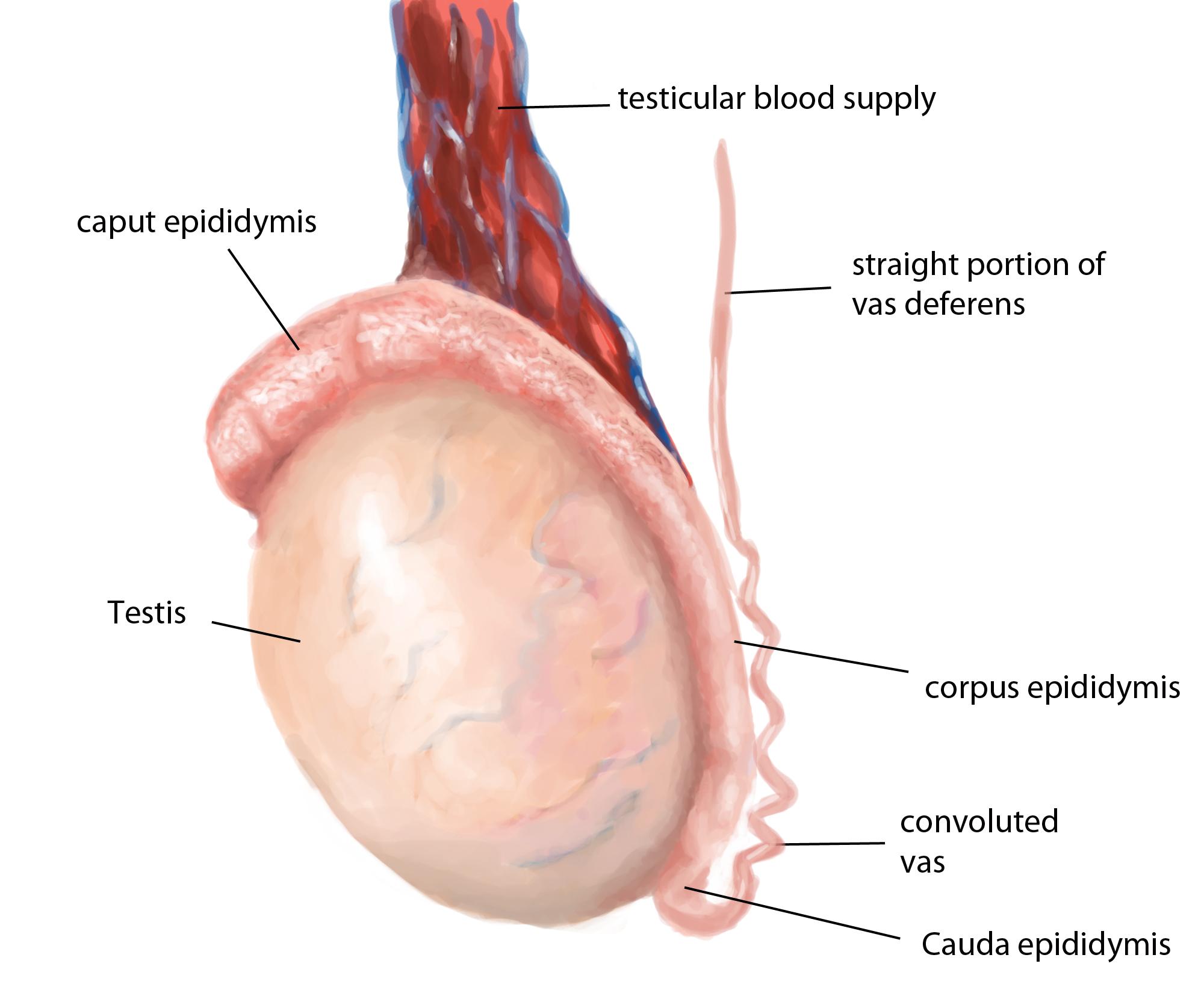
The testicles are a pair of egg-shaped organs located under the penis in men and inside a thin bag called the scrotum. Its task is to produce the male hormone called Testosterone and sperm cells. Testicular cancer is a type of cancer that often arises from testicular reproductive cells. It is frequently seen in young men. It constitutes 1% of male cancers. The incidence of testicular cancer in European countries is 3-10 per 100,000 people.
What are the causes / risk factors of testicular cancer?
The cause of testicular cancer is not known exactly. However, there are some risk factors for testicular cancer. The main ones are:
- Testicular dysgenesis syndrome that includes undescended testis, hypospadias and infertility.
- Testicular cancer risk is 4-8 times higher in patients with undescended testicle.
- A person with testicular cancer is more likely to develop testicular cancer in the other testicle.
- Genetic Factors: Testicular cancer in first degree relatives increases the risk.
How is testicular cancer suspected and how is it diagnosed?
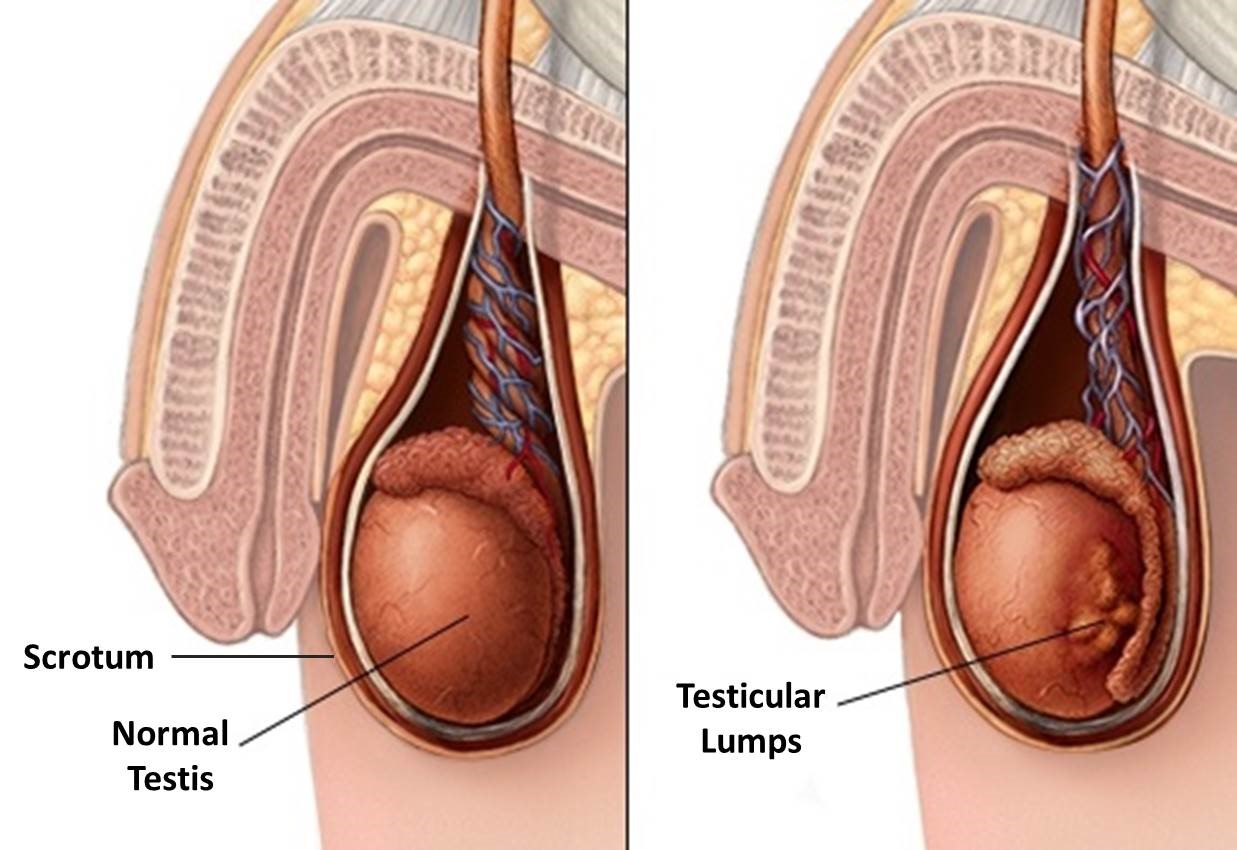
The most important and most common symptom of testicular cancer is painless swelling in the testicle. Testicle is palpable as a hard structure. Rarely, this swelling may be painful. If the tumor in the testicle causes fluid to accumulate in the scrotum suddenly, it may present as a hydrocele on examination.
In case the cancer spreads to the lymph nodes, there may be pain in the back.
Testicular cancer may also complain according to the organ it metastasizes to. For example, chest pain, shortness of breath, and cough may occur if it spreads to the lungs, which is the organ it metastasizes most often.
Scrotal doppler ultrasonography is the first imaging method to be performed in people who have testicular swelling and are thought to have testicular tumor. Ultrasonography can detect masses in the testis with high accuracy.
Chest radiography will help us to evaluate whether there is disease spread in the lung.
Computed Tomography can be used to detect whether the tumor has spread to lymph nodes and other organs in the back of the abdomen.
In addition, some blood values may increase in testicular cancers. Therefore, alpha-fetoprotein (AFP), beta human chorionic gonadotropin (hCG) and lactate dehydrogenase (LDH) levels should be checked before surgery. The high amount of these in the blood suggests testicular cancer. However, just because their amount is normal does not mean that testicular cancer is absent. The level of these hormones is important in postoperative follow-up.
The presence and typing of cancer in the diagnosis can be clearly stated after the surgical removal of the testicle and pathological examination.
Testicular Removal
If there is a suspicion of testicular cancer as a result of the examinations and imaging investigations, the presence and typing of cancer can only be determined by removing and examining the testicle. Thus, the testicular tumor, which is thought to be cancer, should be removed as soon as possible because the growth rate is high. The testis is removed from the inguinal area with an incision (Radical inguinal orchiectomy). Because the lymph of the bag called scrotum and surrounding the testicle goes to different regions from the testicle. Incision or biopsy procedures to be made on the scrotum may cause the testicular tumor to spread to different areas.
How is testicular cancer staged?
Clinical staging should be done before treatment and follow-up planning of testicular cancer. Thus, staging with pathology result, tumor markers (AFP, B-hCG, LDH) measured in the blood, lung films and Computed Tomography is mandatory.
Testicular cancer can occur in 3 stages:
Stage 0: Cancer cells are located only in the thin canals where sperm cells develop and are located. These cells did not spread to normal tissues. This condition, also known as “Carcinoma In Situ”, can also be named as “precancerous condition”. All tumor markers are normal.
Stage I: It is classified into 3 subgroups as Stage IA, Stage IB and Stage IS. This classification is made after the cancerous testicle is removed and examined by radical inguinal orchiectomy.
Stage IA, the cancer is in the epididymis with testicle or in testicle alone. One possibility may have spread to the membrane surrounding the testicle. Tumor markers in the blood are normal.
Stage IB, cancer is confined within the testis and epididymis. However, differently, it has spread to blood and lymph vessels in the testicle (vascular and / or lymphatic invasion) or to the outer membrane surrounding the testicle (tunica albuginea).
Stage IS, cancer can be anywhere on the testicle, but after surgery (after testicle removal) all tumor markers are still high
Stage II: It is divided into three subgroups as Stage IIA, Stage IIB and Stage IIC
Stage IIA, the cancer has spread to lymph nodes in the abdomen. There are 5 or less lymph adenopathy (lymph nodes) that do not exceed 2 cm in size. Tumor markers can be normal or slightly elevated (at S1 level).
Stage IIB, the cancer has spread to lymph nodes in the abdomen. There are 5 or less lymph adenopathy (lymph nodes) that exceed 2 cm in size but do not exceed 5 cm in size. Tumor markers can be normal or slightly elevated (at S1 level).
Stage IIC, cancer has spread to lymph nodes in the abdomen. the size of lymph nodes exceeds 5 cm in size. Tumor markers can be normal or slightly elevated (at S1 level).
Stage III: Stage III is staged in three subgroups as Stage IIIA, Stage IIIB and Stage IIIC.
Stage IIIA, The cancer may have spread to one or more lymph nodes in the abdomen. Cancer has spread to the non-regional lymph nodes or lung. Tumor markers can be normal or slightly elevated (at S1 level).
Stage IIIB, cancer has spread to nonregional lymph nodes or lung. Tumor markers are moderately high (at S2 level).
Stage IIIC, cancer has spread to nonregional lymph nodes or lung. Tumor markers are very high (at S3 level).
What is the Treatment for Testicular Cancer?
Treatment in testicular cancer is planned according to the stage of the disease. Surgery, chemotherapy and radiotherapy treatments can be applied. The recovery rate in testicular cancer is very high and it is pleasing.
Despite the response to the treatment applied in testicular tumors, recurrence may occur. The probability of recurrence is highest in the first 2 years. Therefore, close follow-up of the patient is very important. The risk of cancer in the other testicle of the patient is also increased. Therefore, the patient should examine his testis intermittently.
Removing the cancerous testicle does not affect the reproductive potential and sexual life of the patient. However, due to chemotherapy treatment, reproductive functions and ejaculation may be impaired.
The appearance can be improved by placing a testicular prosthesis in place of the removed testicle.
Treatment of Stage I Testicular Cancer
Treatment in stage I testicular cancer varies depending on whether the cancer is in the seminoma or non-seminoma groups.
In stage 1 Seminomas, close monitoring is obtained if the tumor size is <4 cm and there is no “rete testis” involvement. However, in large tumors or if there is “rete testis” involvement, protective doses of radiotherapy can be given to lymph nodes where cancer often progresses. Alternatively, a single dose of “carboplatin” chemotherapy can be given to reduce the risk of tumor formation in this area.
If stage 1 non-seminomas are not at high risk (no lymphovascular invasion or embryonal carcinoma rate <50%), close monitoring is required. However, 2 cycles of BEP chemotherapy should be given to those with high risk. In patients who are not suitable for chemotherapy, the lymph nodes in the abdomen (RPLND surgery) can be removed. This surgery can be performed by open or laparoscopic method.
Treatment of Stage II Testicular Cancer
Treatment in stage II testicular cancer varies depending on whether the cancer is in the seminoma or non-seminoma groups.
In Seminoma, the following options are considered in treatment.
In stage 2A and 2B seminomas, after the testicle is surgically removed, radiotherapy is applied to the lymph nodes around the main vessels at the intra-abdominal level and also at the bone pelvis (hip bone) level.
In stage 2C seminomas, 3 or 4 cycles of BEP chemotherapy is given according to prognostic factors.
In Non-seminoma, the following options are considered in treatment
In stage 2A and 2B non-seminomas, after the testicle is surgically removed, 3 cycles of BEP chemotherapy is applied if tumor markers are high, and RLND surgery is applied if tumor markers are normal.
In stage 2C non-seminomas, 3 or 4 cycles of BEP chemotherapy is given according to prognostic factors.
Treatment of Stage III Testicular Cancer
Treatment in stage II testicular cancer varies depending on whether the cancer is the seminoma or non-seminoma. The patient is given 3 or 4 cycles of BEP chemotherapy, depending on prognostic factors.
After chemotherapy applications, the remaining lymph nodes in non-seminoma stage 3 cancers where tumor markers regress to normal and large (> 1 cm) lymph nodes are detected surgically (RPLND surgery).
RPLND is a surgery that requires experience and it is recommended that this surgery should be performed in centers where it has been frequently performed before or by experienced surgeons.