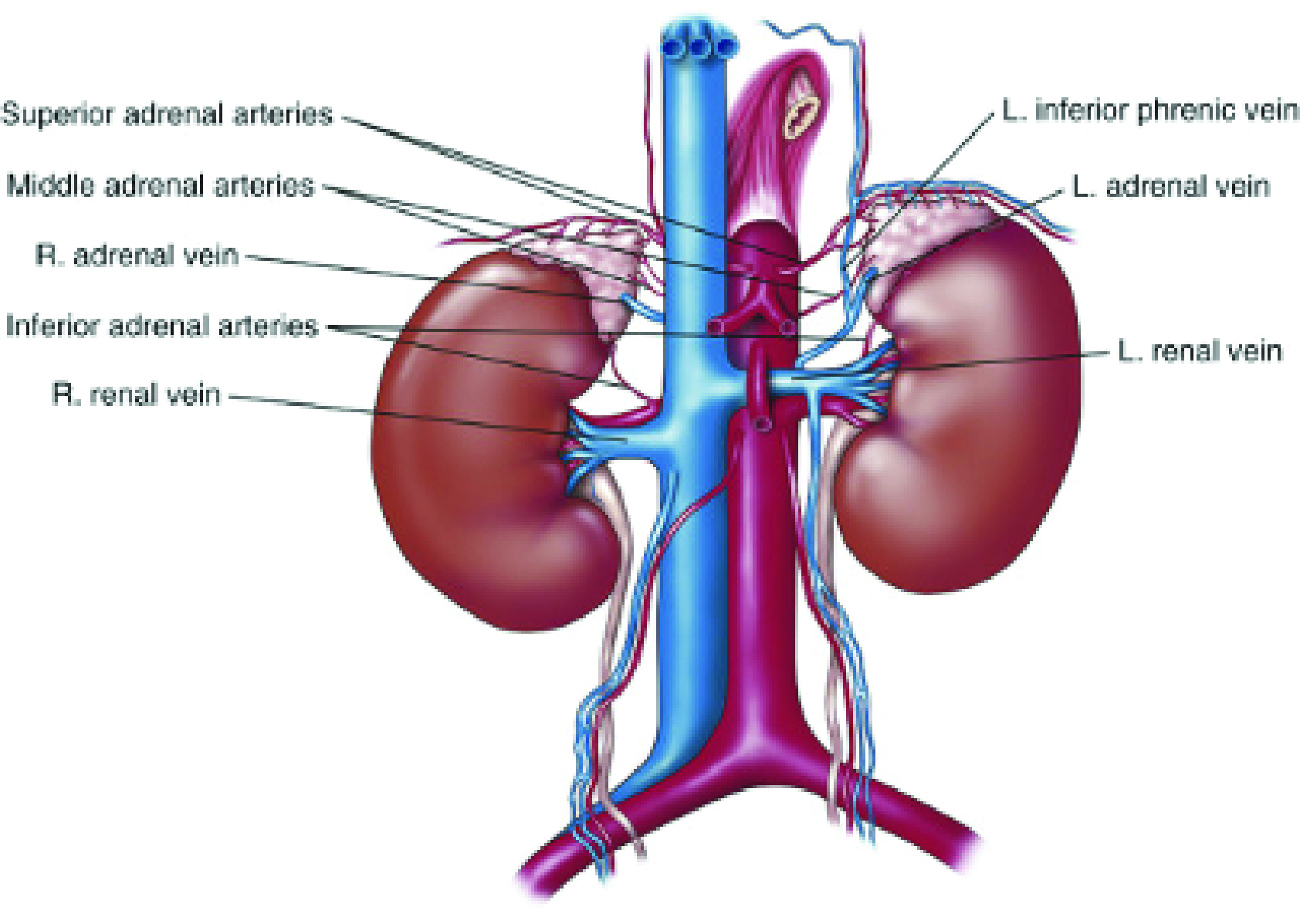
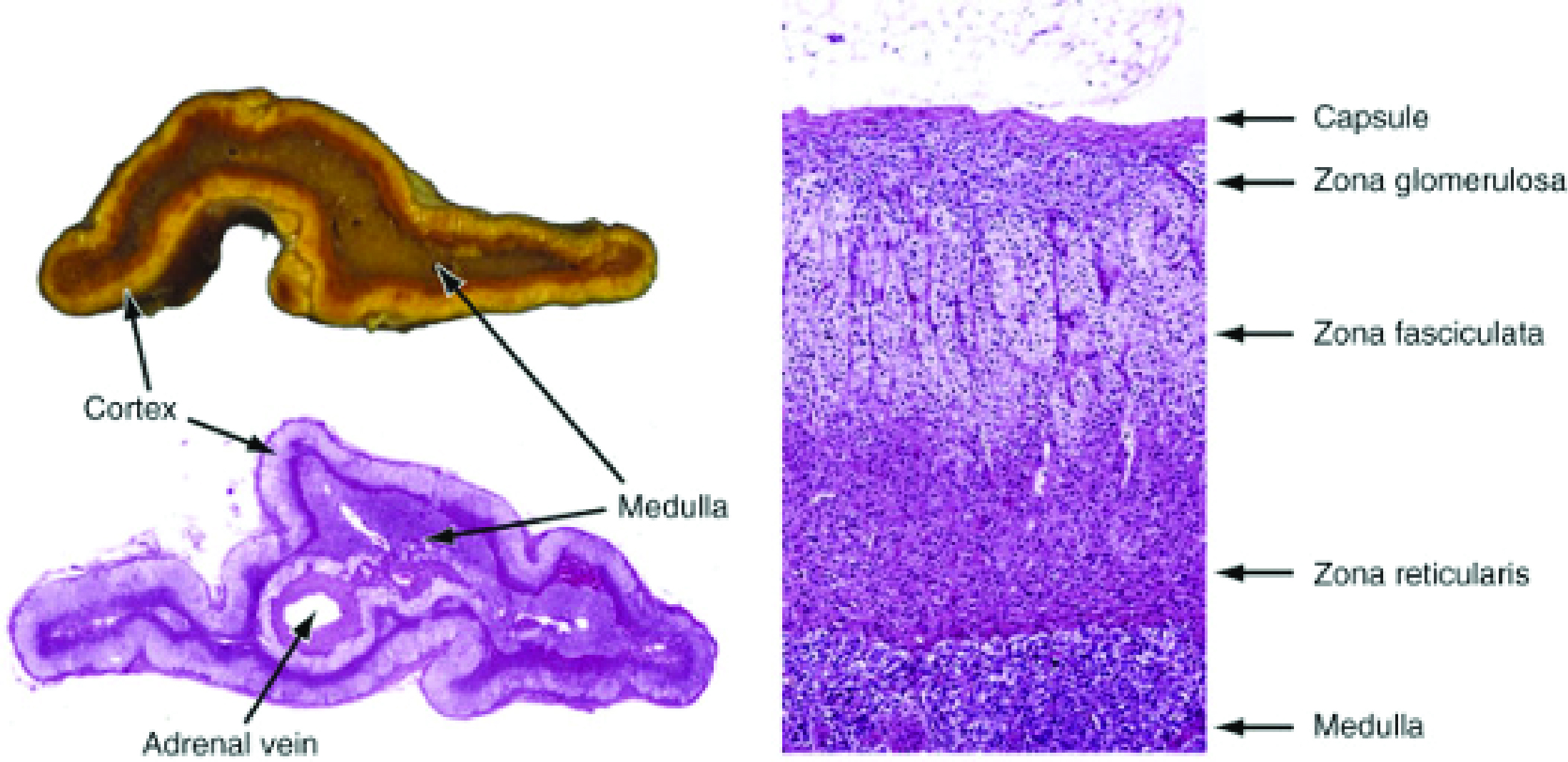
The Zona Fasciculata is the site of glucocorticoid production. In case of excessive secretion, “Cushing Syndrome” occurs.
The Zona Reticularis is the innermost zone of the adrenal cortex and is the part that releases androgens. The deviations during the death of these hormones cause the clinical picture known as “congenital adrenal hyperplasia“.
The Adrenal Medulla which lies at the center of the gland, is an integral part of the autonomic nervous system. Chromaffin cells of the medulla are innervated by preganglionic sympathetic fibers of T11 to L2. For clinical purposes, three metabolites (metanephrine, normetanephrine, and vanillylmandelic acid [VMA]) and two enzymes (catechol- O -methyltransferase [COMT] and monoamine oxidase [MAO]) are important. With the increase of these metabolites, the clinical picture of “pheochromocytoma” occurs.
What is an adrenal incidentaloma? What is its significance?
Adrenal incidence defines adrenal masses found incidentally in imaging tests performed for other reasons. Its frequency in imaging series is reported as 5%. They are often unilateral and most of them are asymptomatic. They are mostly benign.
The retroperitoneal space allows for relatively asymptomatic growth of most adrenal lesions, which may reach huge size before clinically manifesting.
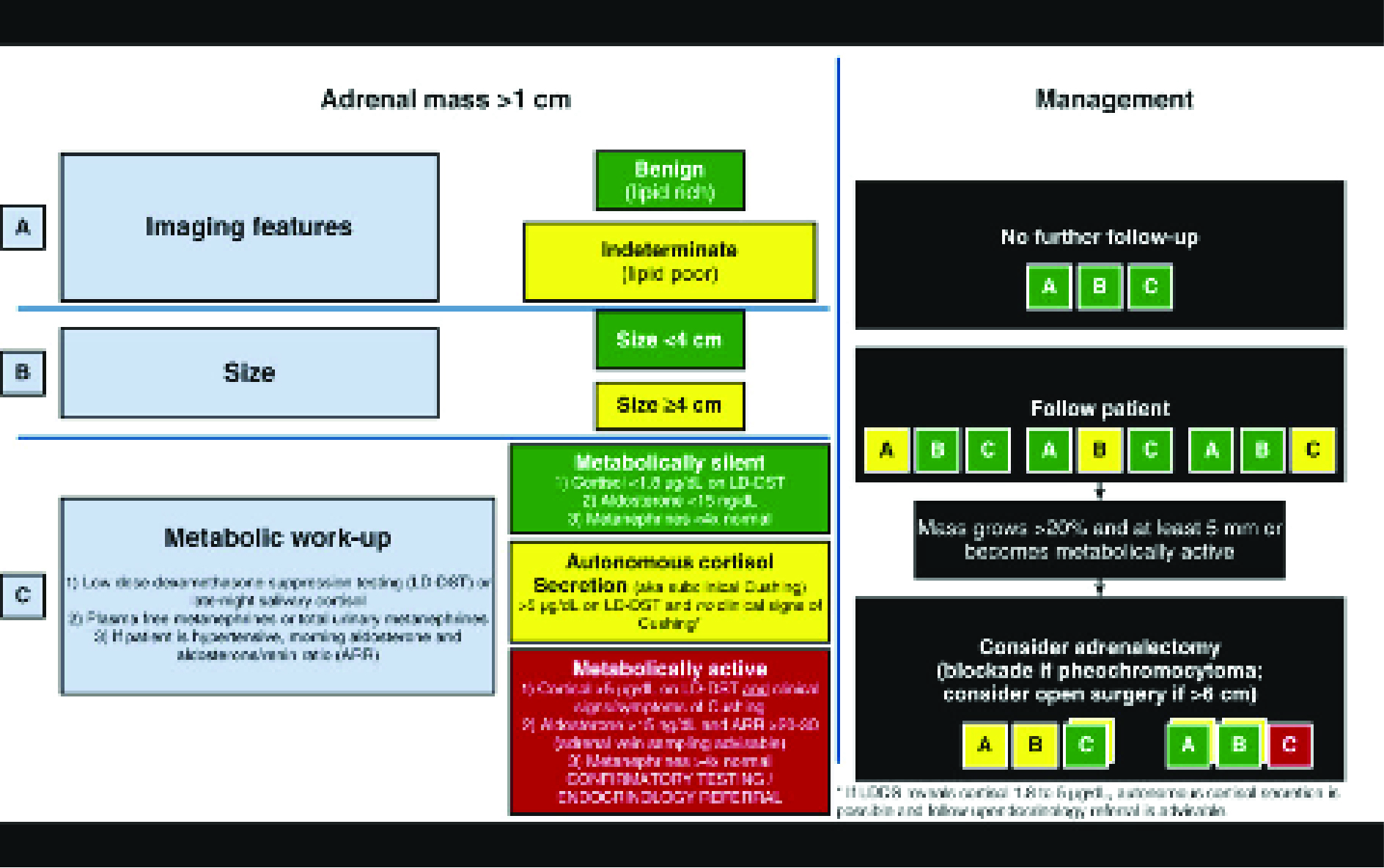
There is a strong relationship between the size of the mass and malignancy (cancer), and the risk of malignancy is low in masses smaller than 4 cm. If it is smaller than 4 cm and non-functional (not producing hormones), it is concluded that it is not malignant (cancer). Masses larger than 6 cm are considered malignant unless proven otherwise. The malignancy rate is 6% in masses between 4-6 cm, and the clinical approach is controversial. Recently, monitoring of 4-6 cm adrenal incidentalomas if non-functional is more accepted.
How should Imaging in Adrenal Masses be?
Ultrasonography is an inadequate imaging method for detecting and characterizing adrenal mass, therefore it is not preferred.
Unenhanced Computed Tomography (CT) can very well evaluate the amount of intracellular fat in more than 70% of adrenal adenomas. However, the mass can be diagnosed with washout levels measured on contrast-enhanced CT in masses with low fat ratio, which constitutes approximately 30% of the segment and cannot be recognized on CT without contrast.
With Magnetic Resonance Examination (MRI), the amount of fat in adrenal incidence can be measured reliably.
Positron emission tomography (PET) with either fludeoxyglucose F 18 (FDG) or 11C-metomidate (MTO) can be helpful in selected patients (eg, those with a prior history of malignancy or those in which unenhanced CT attenuation or washout analysis is inconclusive or suspicious for malignancy) because of their high sensitivity for detecting malignancy
Treatment of adrenal masses
Two points are very important in adrenal masses: the size of the tumor and whether it is functional or not.
Masses <4 cm and non-functional are considered benign.
Follow-up is very important in non-functional masses between 4-6 cm. An increase of more than 20% or at least 5 mm in the size of the mass; or if it becomes metabolically active (functional), the adrenal gland is surgically removed.
Large masses at 6 cm are considered malignant (cancer), even if they are non-functional, and surgical treatment is applied.
Surgery should be performed in hormone-active adrenal masses regardless of its size. These patients may present with clinical findings of Cushing’s syndrome, Conn’s disease, congenital adrenal hyperplasia (CAD) or pheochromocytoma, depending on the type of hormone secreted. A multidisciplinary approach with Urology, Endocrinology and Neurosurgeons when necessary is very important in treatment and follow-up.
Adrenal myelolipoma is a benign adrenal tumor composed of mature fat and interspersed hematopoietic elements that resemble bone marrow. On computed imaging, the presence of large amounts of macroscopic fat in an adrenal mass is diagnostic of a myelolipoma. Although adrenal myelolipomas may grow over time, they can usually be followed without surgical excision. However, when larger than 6 cm in diameter or when causing local mass-effect symptoms, surgical removal should be considered. When adrenal myelolipomas are bilateral, the clinician should consider the diagnosis of congenital adrenal hyperplasia
Adrenal cortical carcinoma may or may not be functional. Unfortunately, most of them are malignant tumors that occur in an advanced stage. Recurrence and metastasis (spreading to other areas) risk is also high in those who are localized. Aggressive wide surgical resection is important in treatment. Therefore, open surgery approach may be more appropriate in locally advanced stage carcinomas. Mitotane therapy is the most commonly used treatment method in adjuvant therapy. Radiotherapy has a very limited place in this disease and can be used in bone and brain involvement.