Kindey Cancer
What is kidney cancer and how does it occur?
Kidney cancer is malignant cell growth within the kidney. Tumors in the kidney can also be benign. Cancer is the name given to malignant tumors. There are different tumor types with different stages in the kidney.
What are the risk factors for kidney cancer? Does genetics play a role?
Although it is not always possible to determine the cause of kidney cancer, smoking and obesity are reported as major risk factors.
Those with kidney cancer in a first-degree relative and those with high blood pressure (hypertension) are at risk for developing kidney cancer.
How is kidney cancer diagnosed?
Kidney cancers constitute about 2% of all cancers. Although the number of kidney cancer patients has increased slightly in recent years, cancer-related mortality rates have decreased in many countries. Kidney cancers are often asymptomatic, meaning there are no specific symptoms that indicate the disease. Most kidney tumors are detected incidentally during routine imaging procedures. However, one in 10 patients may have symptoms such as flank pain and blood in the urine. Sometimes, although rare, conditions called paraneoplastic syndrome can be seen. These are reactions caused by any type of cancer that occurs in the body, such as high blood pressure, weight loss, fever, anemia, loss of muscle mass and loss of appetite. Kidney cancer-associated syndromes often involve liver enzymes and platelet changes. Bone pain or persistent cough may be a sign of cancer metastasis.
It is observed that the rates of early diagnosis have increased due to the advances in imaging technologies such as ultrasound and Computed Tomography (CT) / Magnetic Resonance Imaging (MRI) and frequent use of imaging methods for various reasons. Solid masses in the kidney should be considered malignant (malignant, malignant) unless proven otherwise. The definitive diagnosis and typing of the mass is made by biopsy or pathological examination of the mass removed by surgery.
What are the types of kidney cancer?
Renal cell carcinoma (RCC) is the most common type of kidney cancer. There are 3 subtypes of the RCC:
- Clear cell RCC: It is the most common and the most aggressive. It is often accompanied by the von Hippel-Lindau (VHL) gene mutation on the 3rd chromosome. Apart from this, it is known that SETD2, BAP 1 and PBRM1 tumor suppressor genes, which are located in the vicinity of the VHL gene, are also affected in clear cell RCCs.
- Papillary RCC: It is the second most common subtype. Unlike clear cell RCC, papillary RCC is associated with MET gene mutation. They tend to be more organ-confined compared to clear cell Cancer and often exhibit exophytic growth (outgrowth from the kidney).
- Chromophobe BHK: they are unencapsulated masses. Fuhrman grading is not allowed. Its prognosis is better than the other two.
Benign tumors:
Some tumors in the kidney are not cancer. These are known as benign kidney tumors. The most common benign tumors of the kidney are oncocytoma and angiomyplipoma. The most common treatment approach for these tumors is partial nephrectomy and active surveillance.
Kidney cysts:
They are the most common benign lesions in the kidney. These fluid-filled sacs are located on the kidney and are easily recognized by CT. Cysts can be malignant. In this case, they must be surgically removed.
They are classified from 1 to 4 according to the Bosniak classification. Half of Bosnic type 3 cysts and 90% of Bosniac type 4 cysts are malignant.
What are the prognostic factors?
Anatomical factors: Large tumor size, venous invasion, invasion of the renal capsule, invasion of the adrenal glands, lymph nodes and spread to distant organs are poor prognostic factors.
Histological Factors: Fuhrman grade, subtype, sarcomatoid structure of the tumor, microvascular invasion, presence of necrosis in the tumor and collecting system invasion are important in prognosis.
Clinical factors: general performance of the patient, presence of local symptoms, extreme weakness, anemia, the amount of blood clot cells called platelets, the ratio of neutrophil / lymphocyte cells in the blood, C-reactive protein (CRP) and albumin levels in the blood are important indicators of prognosis.
Molecular factors: BAP1 and PBRM1 gene loss on the 3p chromosome is seen in 90% of clear cell kidney tumors with the worst prognosis and is an important risk factor for tumor recurrence. The prognosis was reported to be worse in those with specific BAP1 mutations.
Kidney tumor biopsy
Needle biopsy with ultrasound or computed tomography can be performed in kidney tumors, but it is not a standard procedure used in diagnosis.
A biopsy is required if:
– Your scan results are not clear enough
– You have a tumor small enough to be treated with active surveillance
– You have a tumor small enough to be treated with radiofrequency ablation or cryoablation
How is kidney cancer staged?
Kidney cancer has different stages. If the tumor is limited to the kidney and has not spread, it is called localized kidney cancer. In locally advanced kidney cancer, the tumor has grown out of the kidney into the surrounding tissue and extended to the veins, adrenal gland and lymph nodes. Metastatic disease is mentioned if it has spread to distant lymph nodes or other organs.
T-1: Tumors <7 cm limited to the kidney
T1a: Tumor smaller than 4 cm limited in the kidney (not exceeding the kidney capsule)
T1b: Tumor limited to the kidney (not exceeding the kidney capsule) with a size of 4-7 cm
T-2: Kidney limited masses> 7 cm
T2a: Tumor limited to the kidney (not exceeding the kidney capsule), larger than 7 cm but smaller than 10 cm
T2b: Tumor diameter greater than 10 cm and not exceeding the kidney capsule
T-3: Locally advanced tumors
T3a: Tumor that has spread to the renal vein or its branches; or tumor extending into perirenal adipose tissue but not exceeding gerota
T3b: Vena cava inferior involvement below the level of the diaphragm
T3c: Vena cava inferior involvement above the level of the diaphragm, or tumor invasion of the vena cava Wall
T-4: The tumor has exceeded the membrane surrounding the adipose tissue (Gerota fascia) around the kidney.
Lymph Nodes:
Nx: Regional lymph nodes not evaluated
N0: No tumor spread in regional lymph nodes
N1: There is tumor spread in regional lymph nodes.
Distant Metastasis:
M0: Cancer does not spread to distant organs
M1: Cancer has spread to distant organs.

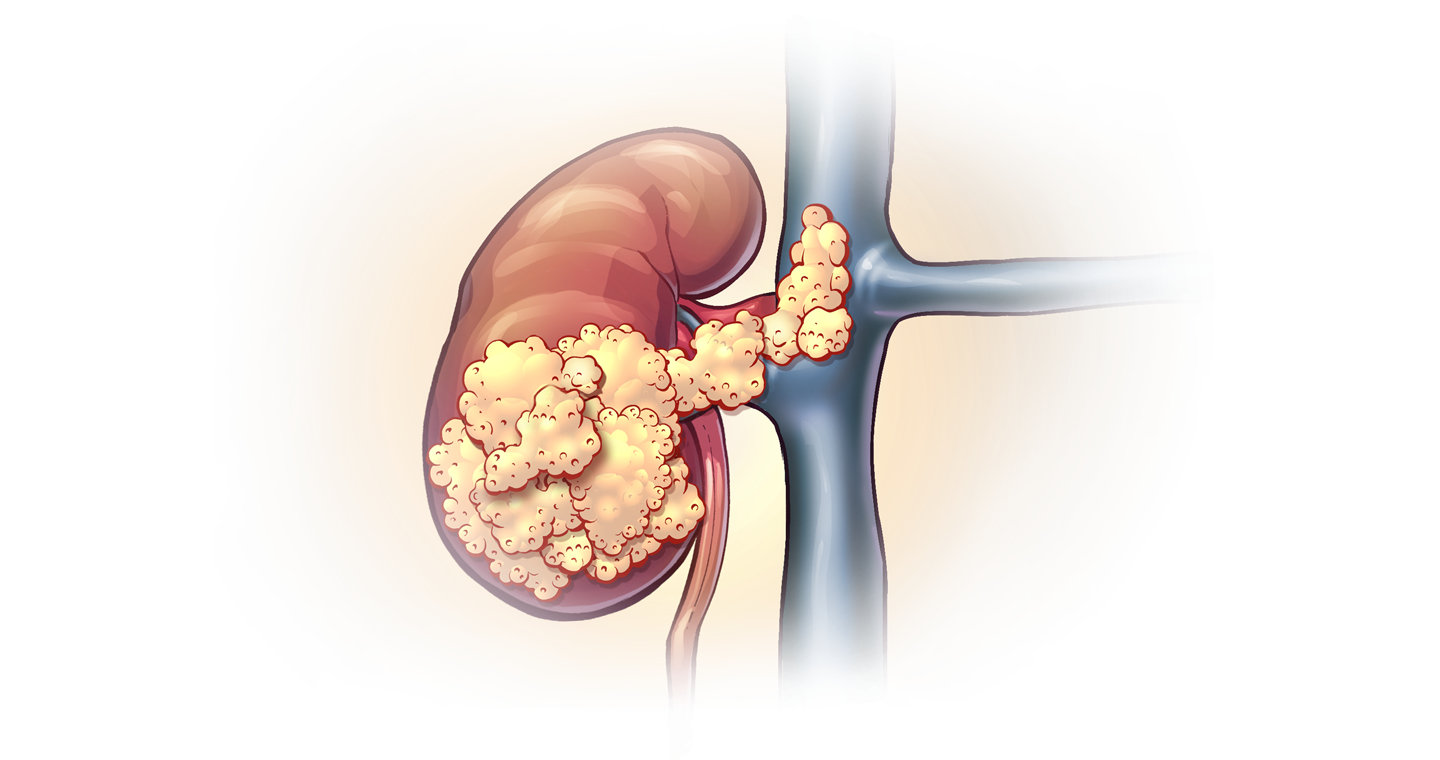
What is locally advanced kidney cancer?
It means that the tumor has spread to the blood vessels, fatty tissue, organs and lymph nodes around the kidney. It can be called stage III or IV and shows how far the tumor has spread.
How is support and treatment in kidney cancer?
Surgical approach is the most appropriate to cure localized kidney cancers. Partial nephrectomy (removal of the tumor area by preserving the kidney) should be performed in tumors of suitable size and location. In T2 (> 7 cm) tumors or in patients whose localization is not suitable for partial nephrectomy, radical nephrectomy (removal of the kidney and surrounding tissues) is performed. Radical / Partial nephrectomy can be done by laparoscopic or open methods.
In locally advanced kidney cancers, it is recommended to remove the lymph nodes if lymph node involvement is detected. In vena cava thrombi, the thrombus should be removed together with the tumor kidney.
If surgery is impossible or has high risk for patient, embolization (the feeding of cancer cells is disrupted by closing the arteries leading to the tumor) may be recommended.
Active surveillance may be recommended especially in elderly patients in the presence of small kidney tumors (<4 cm). Studies have shown that when small masses are monitored, the tumor metastasizes in only 1% of patients. During the active surveillance period, the tumor is monitored with regular imaging procedures. If the tumor continues to grow, additional treatment may be required. In this case, ablation (radiofrequency- or cryo-) therapy may be a good alternative.
Ablation therapy can be performed by radiofrequency ablation (RFA) or cryotherapy. With these processes, it is aimed to kill tumor cells by heating (RFA) or freezing (cryotherapy).
Cancer diagnosis has a serious impact on the lives of patients and their relatives. It can lead to anxiety, fear and depression; It can affect your work and social life. When patients need support, they should share this with their doctor.

Help with daily activities may be needed during the first day or weeks after surgery. Patient attendant may be important in the first days after surgery.
The follow-up protocol should be planned according to the pathology and stage in the postoperative controls.
It is important to continue your lifestyle during and after treatment. Try to eat a balanced diet consisting of vegetables, fruits and milk. Try to quit smoking. It can help you recover faster after surgery.
Is there any risk of the treatment?
Radical nephrectomy is a common procedure in the treatment of locally advanced kidney cancer. Since the patient is left with a single kidney after surgery, the risk of chronic kidney failure increases, especially in patients with additional diseases such as diabetes (diabetes) and hypertension. In addition, possible decreased kidney function after surgery poses a risk for cardiovascular diseases.
As in all major surgeries, it also contains general risks of anesthesia.
How should the follow-up be and what should be considered?
A follow-up protocol should be established according to the clinical and pathological stage after surgery. It is also very important to protect health during and after treatment, and regular physical exercise for the purpose and quitting smoking if used will reduce the risk of tumor development.
It is recommended to eat a balanced diet that includes vegetables, fruits and dairy products. Starchy meals such as bread, potatoes, rice and pasta and protein-rich foods such as meat, fish and eggs should be consumed. However, sugary, salty and fatty meals should be avoided as much as possible.
After treatment, the prognosis of the disease may cause concern. We often see the fear of cancer recurrence in patients. If this situation creates anxiety and fear in you, you may need psychological support.

Palliative care for kidney cancer
Palliative care is a care that aims to improve the quality of your life when there is a disease that cannot be cured and can be done at home or in a hospital.
We also encounter situations where it is not possible to recover from kidney cancer. When the applied treatment is not successful for a longer time, palliative care is recommended to increase patient comfort.
Metastatic Kidney Cancer
Kidney tumors can spread to other organs or lymph nodes. This is called metastatic disease. Kidney tumor is called primary tumor and tumors in other organs are called metastases. Kidney cancer metastasis usually spreads to the lungs, bones, distant lymph nodes, or brain. Metastatic disease may be asymptomatic or cause different symptoms depending on where the cancer has spread. In lung metastases, there may often be a persistent chronic cough or bone pain in the case of bone metastasis.
In the treatment of metastatic disease, he may recommend a combination of antiangiogenic therapy, known as target therapy, with surgery. In rare cases, immunotherapy can be used.
Risk stratification in Metastatic Kidney Cancer
MSKCC (Memorial Sloan Kettering Cancer Center) prognostic system is used to create risk classes. This classification is determined by the patient’s performance status (Karnofsky performance status <80), time between diagnosis and treatment (<12 months), blood lactate dehydrogenase (LDH) and blood calcium levels (> 10 mg / dl), blood hemoglobin (anemia) and neutrophil levels. Patients are divided into good, moderate and poor prognostic risk classes.
Treatment Options in Metastatic Kidney Cancer
If there is metastatic disease, surgical removal of the kidney (cytoreductive nephrectomy) is recommended to reduce tumor burden and alleviate symptoms. The results of the CARMENA study showed that while cytoreductive nephrectomy prolongs survival significantly in patients in the good-risk group, it does not benefit survival in patients in the moderate and poor-risk groups.
If the metastasis causes too much pain or other symptoms, additional surgery may be required to remove these metastatic tumors. Cytoreductive partial nephrectomy can be performed in patients with a single kidney or where the primary tumor is not too large and the other kidney is not working. In metastatic disease, surgery is combined with medication.
Radiotherapy may also be recommended for the treatment of metastasis. However, kidney tumors generally do not respond to radiotherapy. Therefore, it can only be recommended to relieve symptoms caused by a primary tumor or metastasis that cannot be surgically removed. Despite all these, the role of stereotactic body radiotherapy, which can be given in several fractions, by using high doses per fraction in oligometastatic disease or in the treatment of primary tumor, and radiotherapy in renal cell carcinoma have gained importance.
Usually, metastatic disease cannot be cured. Treatment of metastatic disease is aimed at reducing the size of the primary tumor and metastases. This will give the patient the chance of a longer life and less symptoms. These are general information and treatment differences may occur for each patient.
Chemotherapy is also not a very effective treatment option for kidney cancer. Combined immunotherapy with 5-fluorouracil may be effective after complete resection (complete removal) of the primary tumor in metastatic tumors.
Immunotherapy is one of the drug treatments used in metastatic kidney cancers. Immunotherapy is a type of treatment that strengthens the immune system to combat tumor cells. 2 different immunotherapy can be used in metastatic kidney tumors.
– Interferon-alpha (INF-α)
– Interlokin-2 (IL-2)
Antiangiogenic treatments are the most commonly used drug treatments in metastatic kidney cancers.
The patient may be recommended preoperative drug therapy to shrink the tumor. In some cases, antiangiogenic therapy is used before surgery to see how the cancer will respond to this. If a good response is obtained, treatment is continued after surgery. If surgical treatment is not possible, drug treatments are started. Generally, antiangiogenic therapy, which acts on tumor growth by preventing the formation of blood vessels, is preferred.
Antiangiogenic Therapy
These treatments are arranged and applied by a medical oncologist. However, treatment and follow-up with a multidisciplinary approach is very important in kidney cancers.
Antiangiogenic (tyrosine kinase inhibitors and monoclonal antibodies) drugs commonly used in kidney cancer treatment:
-Sunitinib -Pazopanib -Axitinib -Sorafenib -Tivozanib -Bevacizumab
mTOR inhibitor drugs aim to shrink the tumor by attacking the enzyme. mTOR is a serine / threonine kinase from the TOR (target of rapamycin) protein family. With mTOR inhibition, both mRNA translation of proteins that work in the cell cycle decreases and HIF-1α translation decreases. There are 2 agents that inhibit this pathway:
-Temsorulimus -Everolimus
Fatigue and nausea are common side effects during these treatments. There may also be diarrhea and constipation. You may have high blood pressure during treatment. While taking these medications, you may experience shortness of breath, chest pain, and swollen ankles and feet. It can also cause clot formation, increasing the risk of heart attack and stroke. You may have dryness, redness or a rash on your skin. In some cases, the skin may turn yellow and improve after treatment is over. You may experience numbness and tingling in the fingers and toes. During the treatment, your hair may turn gray. Some colors may come back between treatment sessions. Blisters and rashes on the palms and soles (hand foot syndrome) may develop or a bitter taste sensation may occur in the mouth.