BLadder Canner
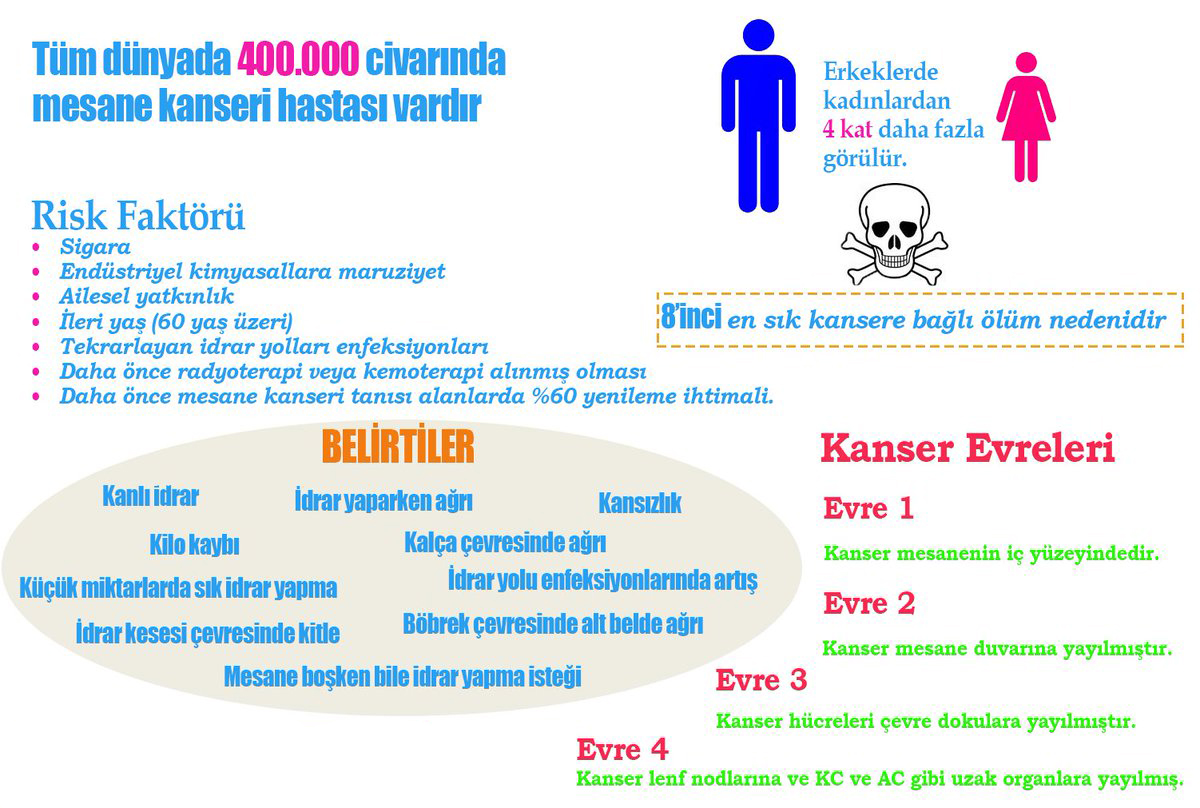
What is the frequency of bladder cancer?
Bladder cancer is the second most common genitourinary cancer in Turkey. It is the 7th most common malignancy in men. In women, it is among the top 10 malignancies and breast cancer, which can be described as a distant relative of bladder cancer, takes the first place. According to the SEER database in the United States, the average incidence of bladder cancer is 72 years.
Does genetics play a role in bladder cancer?
Bladder cancer is one of the most mutagenic cancers known. While there is mutation in 7 oncogenes in low-grade Ta tumors, different mutations, mainly gene amplification and point mutation, were detected in 13 oncogenes in muscle invasive bladder cancer.
In addition, there are different types of mutations in tumor suppressor genes, especially inactivating mutations. In tumor suppressor genes, 13 mutations in low-grade Ta tumors and 17 in muscle invasive tumors were detected.
Low-grade papillary cells are thought to result from hyperplasia. H-RAS and FGFR-3 oncogenes have been shown to be effective in the development of this variant. In general, their potential for multifocality, recurrence and muscle invasion is limited.
In the development of invasive tumors, it has been shown that mutations in the p53 and retinoblastoma (rb) tumor suppressor genes are the most common.
After 2015, bladder cancer is examined under two headings as “basal” and “luminal” at the end of genetic / molecular examinations.
Basal type bladder cancer
1- It has a poor prognosis. Basal molecular type is more common in muscle-invasive cancers in women. Perhaps this is one reason for the poor prognosis of bladder cancer in women.
2- Sarcomatoid and squamous differentiations which were associated with poor prognosis are more common
3- Claudin family gene expressions associated with good prognosis are less common
4- Expression of late cell cycle genes associated with tumor aggressiveness is observed.
Luminal type bladder cancers:
1- It is associated with papillary histology.
2- Urothelial differentiation markers associated with good prognosis are expressed.
3- Expression of early cell cycle genes associated with good prognosis is seen.
4- It has estrogen receptors.
Survival times are longer in luminal type bladder cancer than in basal type table cancers. However, basal type bladder cancer is more sensitive to chemotherapy.
However, there is no easy and cheap laboratory analysis that can distinguish luminal and basal types in the clinic.
What are the risk factors for bladder cancer?
Due to the “aromatic amines” and “policyclic aromatic hydrocarbon” it contains, smoking is known as the strongest risk factor for bladder cancer today. Smoking is detected in half of the patients with bladder cancer.
Workers in the oil, metal, and paint industries are also at risk of developing bladder cancer due to exposure to “aromatic amines”, “policyclic aromatic hydrocarbon” and “chlorinated hydrocarbon”.
Radiation exposure increases the risk of bladder cancer. Schistosoma which is a rare bladder infection in Turkey also increases the risk of bladder cancer.
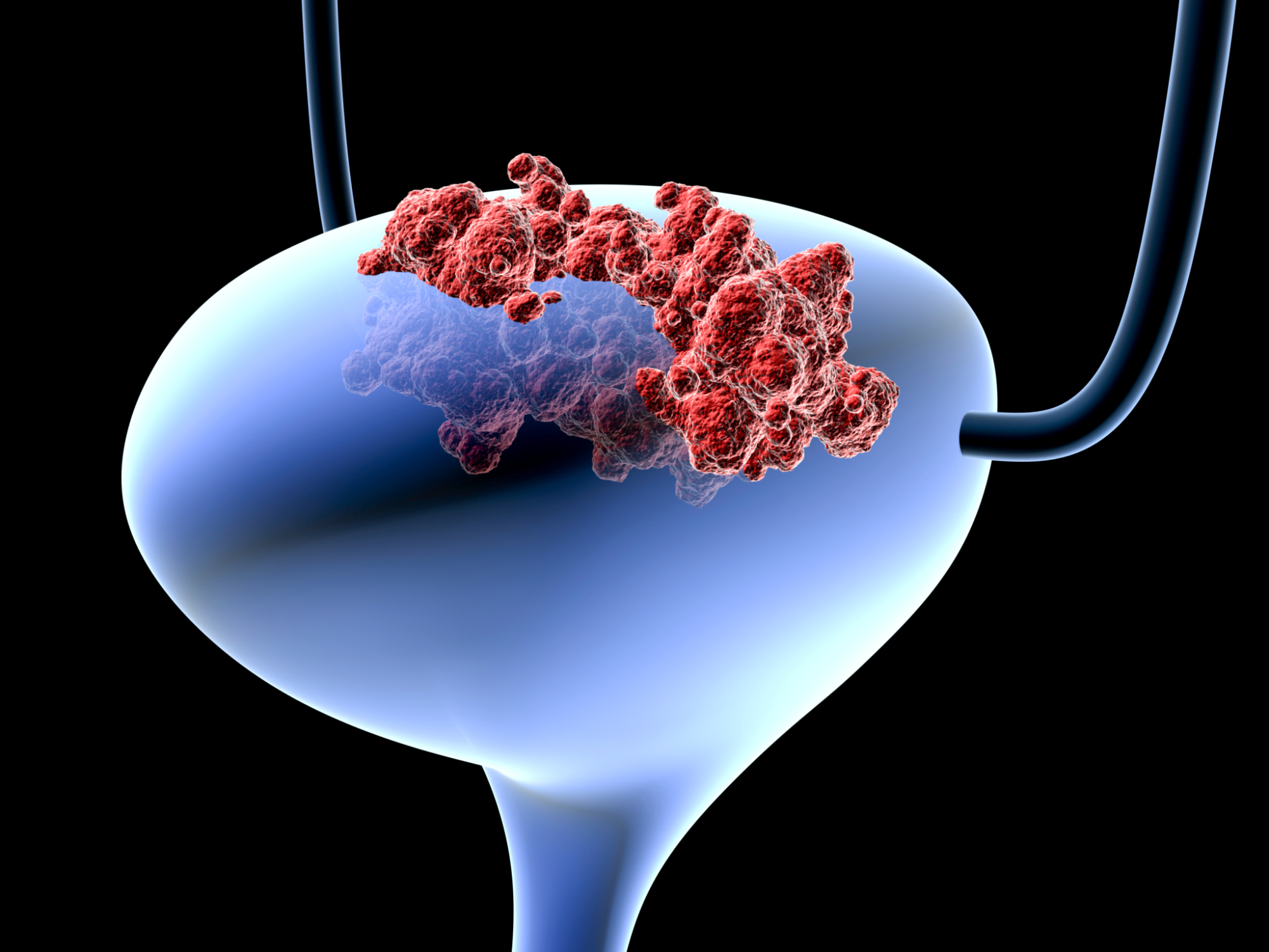
How is bladder cancer suspected and how is it diagnosed?
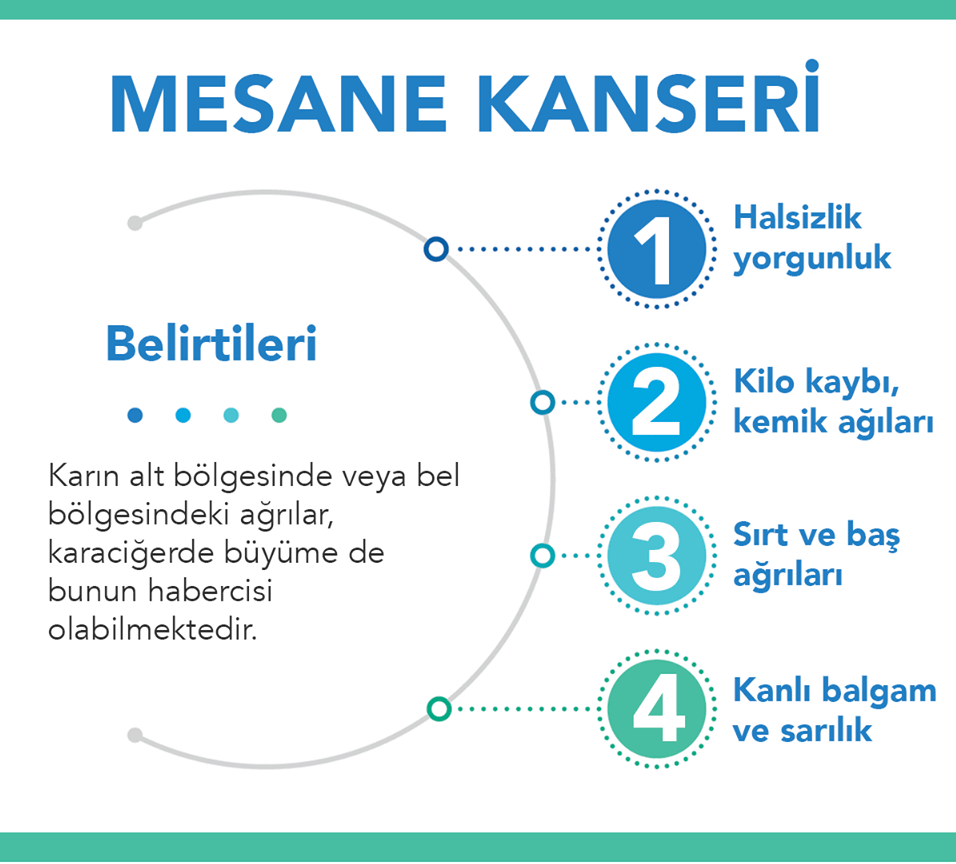
While bladder cancer often presents with urinary bleeding (hematuria), it can also be detected incidentally by imaging methods. Urinary system scanning is performed with imaging methods such as ultrasonography / IVP / CT (Computed Tomography) / MRI in the patient presenting with hematuria.
Urine cytology (searching for spilled tumor cells in microscopic examination of urine sample) is a valuable method with a specificity of up to 90%, especially in high grade tumors. However, its diagnostic value (sensitivity) is low in low grade tumors (16%).
If the bleeding focus cannot be detected by imaging methods after excluding other causes that may cause bleeding, it is useful to perform diagnostic cystoscopy. Because we have the opportunity to detect superficial bladder tumors by cystoscope rather than imaging methods. Biopsy taken from suspicious areas in cystoscopy will give the opportunity to make a definite pathological diagnosis.
A mass to be detected in cystoscopy will be resected in the same session (TUR-BLADDER surgery), which will enable us to diagnose pathologically, perform pathological staging, and curative treatment in some patients.
Although urine markers such as FISH, microsatellite analysis, and NMP-22 have begun to be used in tumor screening in recent years, new investigations are needed.
How should the approach be for a newly diagnosed bladder mass?
If a mass is detected in the bladder, the mass should be completely resected (all masses in the bladder should be scraped). Carcinoma in situ (CIS) is the pathology with the worst prognosis in non-muscle invasive bladder cancer. It has been reported that CIS is detected in the prostatic urethra in approximately 11.7% of bladder cancers, and biopsy from the prostatic urethra is recommended in risky patients. These risk factors are:
- Tumor in the bladder trigon or bladder neck
- Cases with CIS in the bladder
- Those with multiple tumors
Another important issue after TUR-B in bladder cancer is re-TUR-B, in other words, the process of scraping the tumor bed again in a second session. Studies have shown that when TUR-M was applied again to patients with pathology stage “T1”, 33-55% and 41.4% of patients with “TaG3” had residual rest tumors. That’s why TUR-B should be repeated in the following cases:
- In tumors undergoing incomplete TUR-M (which cannot be completely resected in one session due to the size of the mass)
- Tumors whose muscle tissue is not sampled in tumor examination
- In pathological stage T1 tumors
What are the sub-types of bladder cancer?
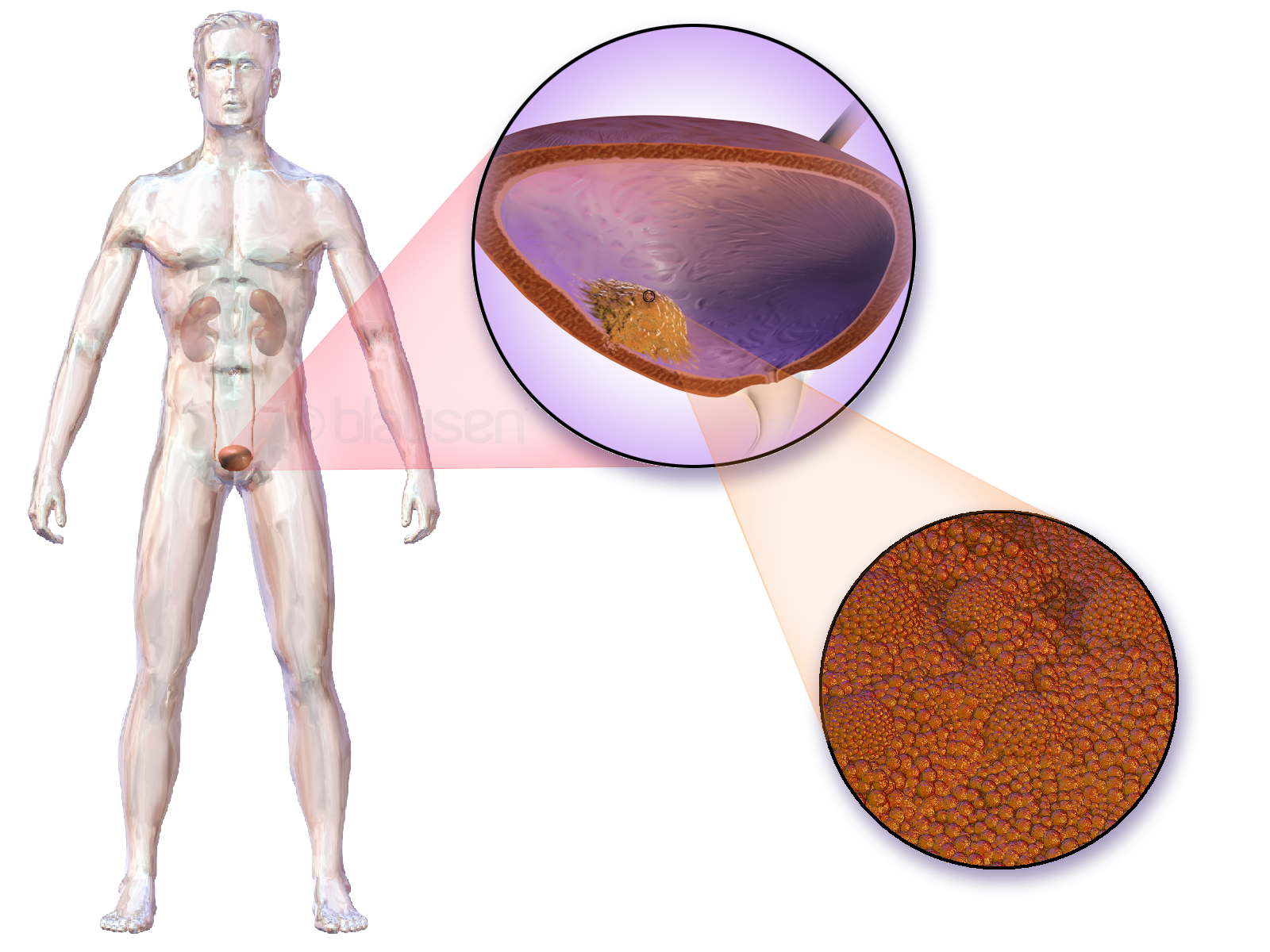
Transitional epithelial cell carcinoma (Uroepithelial carcinoma): In this type of cancer, cancer arises from cells that line the inner surface of the bladder, called epithelial cells. It is the most common type of bladder cancer. More than 90% of bladder cancers are these types of tumors. The bladder can be in a single and papillary form, or it can be widespread and solid in the bladder.
Squamous cell carcinoma (Squamous cell carcinoma): Cancer arises from squamous cells (squamous cells) in the bladder with prolonged exposure to infection and irritation of the bladder. Approximately 6-8% of bladder cancers consist of this type of cancer.
Adenocarcinoma: This type of cancer arises from glandular (secretory, secretory) cells in the bladder. These secreting glandular cells line the bladder wall and provide mucus production. Approximately 2% of bladder cancers are this type of cancer.
How is bladder cancer staged?
The first thing to do in a patient with a mass detected in the bladder is to make a tissue sample using TUR (Trans Uretral Resection) method. Especially in muscle invasive bladder cancer, clinical staging with imaging methods should be done together with pathological staging.
TNM classification system is used in staging. T: tumor; N: lymph nodes; M: represents distant metastasis.
Tx: Tumor presence not evaluated
T0: No evidence of tumor presence
Tis : Carcinoma in situ
T1 : Tumor has advanced to subepithelial tissue
T2: Muscle invasive tumor
T2a : Superficial muscles involved (half facing into the bladder)
T2b : Deep muscles are involved (half facing the bladder floor)
T3: Tumor has advanced to perivesical tissue
T3a: microscopically
T3b: macroscopically (a mass outside the bladder)
T4: The tumor has advanced to either of the prostate stroma, seminal vesicle, uterus, vagina, pelvic wall, abdominal wall.
T4a: Tumor is invasive in prostate stroma, seminal vesicle, uterus or vagina.
T3b: Tumor invases the pelvic wall or abdominal wall
T4: Tumor has spread to adjacent organs other than the seminal vesicle
Nx: no sampling from regional lymph nodes
N0: No tumor in regional lymph nodes
N1: There is a tumor in a single lymph node in the pelvis.
N2: Tumors in many lymph nodes in the pelvis
N3: tumor in common iliac lymph node
M0: No metastasis
M1: Metastasis
M1a: Non-regional lymph node metastasis
M1b: Other distant metastases
What are the risk factors for recurrence and progression in bladder cancer?
One of the most important risk factors for recurrence and progression in bladder cancer is the progression of the cancer to the detrusor muscles of the bladder. The number, size, pathological grade of the tumor such as the stage of the tumor, whether it is the first diagnosis and the accompanying CIS (carcinoma insitu) are important factors affecting recurrence and progression.
Especially CIS is very important in terms of prognosis in non-muscle invasive bladder cancers.
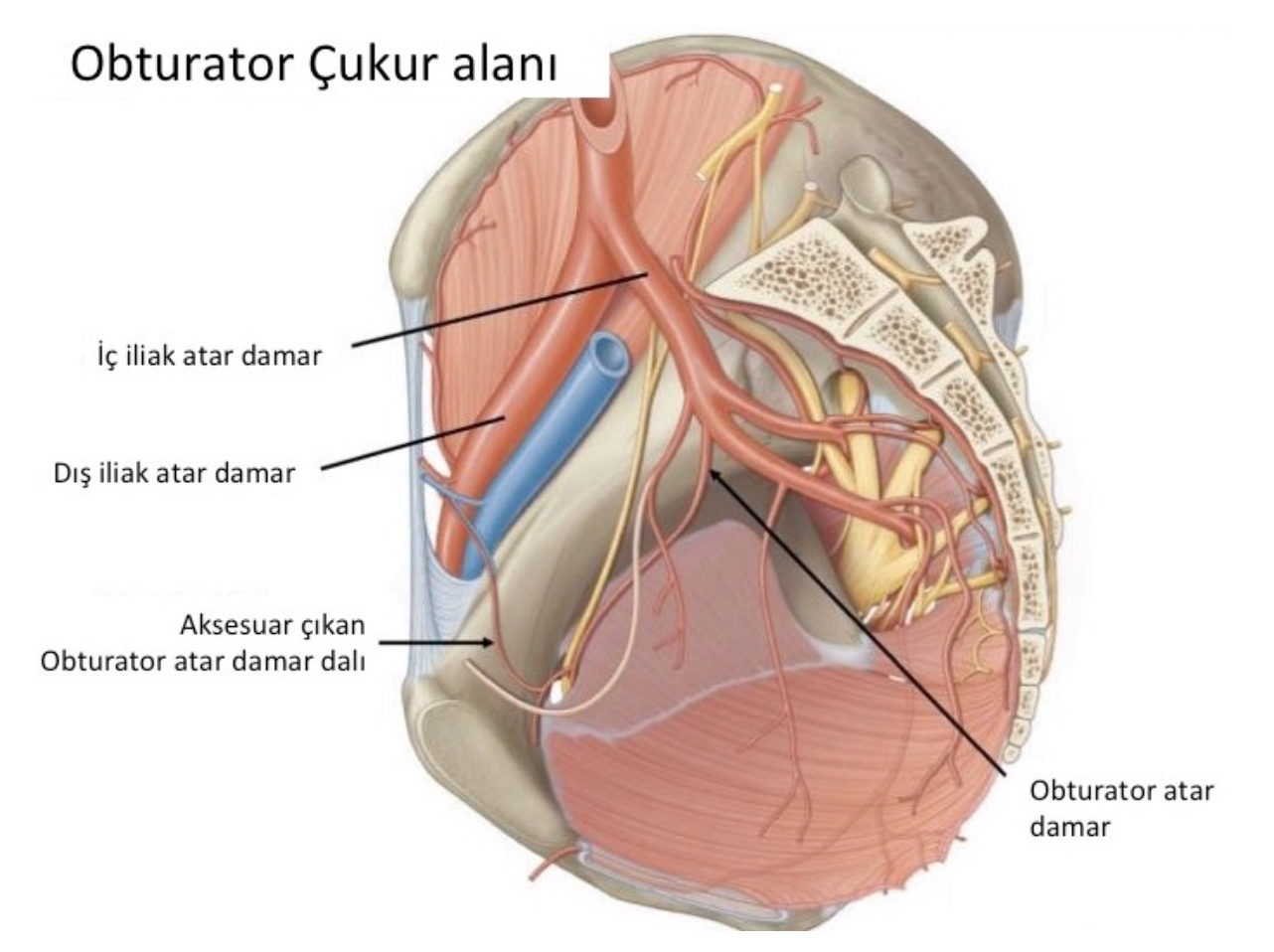
In muscle invasive bladder cancers, the location of the bladder at the base of the bladder, which we call the trigon, increases the likelihood of lymph node involvement and decreases survival.
Why is muscle-invasive bladder cancer important?
It is the most important parameter in terms of prognosis, and its progress to lymph nodes dramatically reduces survival.
How is the treatment in bladder cancer?
We shape our treatment decision by dividing bladder cancers under two main headings as pathologically muscle invasive (advanced to the muscles of the bladder) and non-muscle invasive.
Treatment in non-muscle invasive bladder cancer:
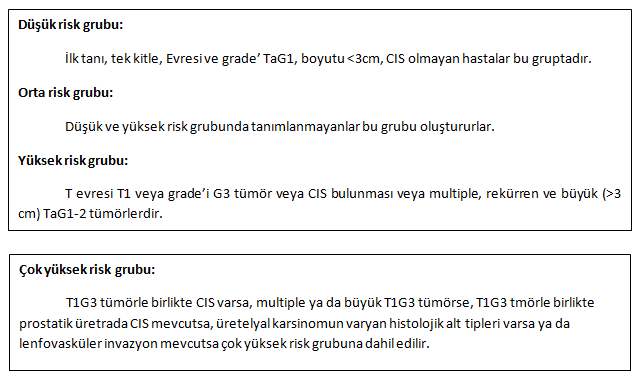
Non-muscle invasive bladder cancers are divided into low, intermediate and high risk groups and include different treatment approaches according to these risk groups.
In non-muscle invasive bladder cancers, removal of the tumor with TUR procedure can completely purify the patient from the tumor, and it often recurs or progresses in stages. Therefore, it is often necessary to add adjuvant therapy.
The possibility of recurrence and progression is low in patients in the low risk group, and intravesical chemotherapy is sufficient in the patient bed immediately after the operation. It is followed up with cystoscopy controls in the 3rd month and 1st year following the TUR surgery.
If the patients in the intermediate risk group have low expectation of recurrence (patients with an EORTC recurrence score of <5), intravesical chemotherapy (into the bladder) in the patient bed immediately after the operation is sufficient. Others are given 1 year intravesical chemotherapy or BCG. While BCG is administered weekly for 3 weeks in the 3rd, 6th and 12th months, chemotherapy still has no optimal standardization.
In patients in the high risk group, BCG application into the bladder from 1 to 3 years and cystoscopy follow-up with 6-month periods for the first 2 years and 3 months after the 5th year.
Radical cystectomy surgery should be recommended for patients in the very high risk group. In patients who are not suitable for radical cystectomy or do not accept it, 1-3 years of intravesical BCG treatment can be applied.
Radical cystectomy is the first choice treatment option in BCG-resistant bladder cancer.
Treatment in muscle invasive bladder cancer:
The most appropriate treatment option in muscle-invasive bladder cancers is complete removal of the bladder with a more radical approach. This procedure is called “Radical Cystectomy”. Urinary diversion is performed with radical cystectomy. The best alternative today for storing urine after the bladder is removed is to reconnect it to the urinary tract by making a new bladder from a part of the small intestine. This surgical procedure is called “Orthotopic Neobladder Reconstruction / Ileal Neobladder Reconstruction”.
In patients who are not suitable for neobladder or with doctor / patient preference, ileal conduit (mouthing the nascent bladder to the anterior abdominal wall) is also used in urinary diversion. Although many parts of the gastrointestinal system can be used in urinary diversion during this surgery, it is the ileum part of the small intestines (also the most preferred in our own clinic). In addition, lymph nodes up to the abdominal aorta level are routinely removed.
What awaits patients after bladder removal?
In patients to be treated with ileal conduit, discharge of urine into the bag on the anterior abdominal wall causes hesitations in the decision-making process of the patients, but we observe that patients get used to it very quickly in our daily practice. Electrolyte disturbances can be seen immediately after surgery, especially in patients who undergo orthotopic neobladder. In addition, it takes 1-2 years for the neobladder to reach its maximum capacity, and urinary incontinence is frequently observed in patients during this process.
Is there a place for chemotherapy in bladder cancer?
Adjuvant chemotherapy is recommended for patients with stage T3-4 or lymph node tumor after radical cystectomy.
Although there is no alternative to this surgery in patients who are not suitable for radical cystectomy surgery, it is applied in combination with radiotherapy.
Chemotherapy is our only treatment option in metastatic disease.