What are the treatment options in prostate cancer?
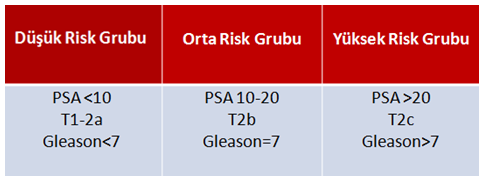
Treatment of prostate cancer varies according to the stage of the disease.
In localized (limited to prostate) prostate cancer, radical prostatectomy surgery, radiotherapy or radiotherapy + androgen deprivation therapy for a limited time is decided by talking to the patient according to the risk groups.
Due to the slow course of cancer, “delaying treatment” called “active surveillance” is another alternative. For this aproach, patient selection and compliance with follow-up is extremely important.
Focal therapies in localized cancer can also be applied, although the level of recommendation is low.
In locally advanced (overflowing from the prostate but not spreading to other organs) prostate cancer, radical prostatectomy surgery or radiotherapy + 2-3 years of LHRH analogue treatment is preferred.
Orchiectomy (removal of both testicles) or LHRH analogue combination is used in metastatic disease.
In metastatic disease, it has now been shown that orchiectomy or LHRH analogues with chemotherapy prolongs the life expectancy by an average of 13 months. Local treatment with radiotherapy or surgery in low-volume metastases and radiotherapy for metastases have also been among the applications of treatments in recent years.
Why are the testicles of the patient removed in metastatic cancer?
Prostate cancer is a “testosterone” dependent cancer. Testicles, the main source of testosterone in the body, are removed to slow cancer. With this treatment, the cancer becomes silent for approximately 24-36 months. However, cancer cells find molecules other than testosterone to reproduce at the end of this period and the disease is defined as “castration resistant” after this stage.
As with orchiectomy, very low testosterone levels can be achieved with LHRH analog/antagonist drugs without removing the testicles. These drugs inhibit the production of testosterone from testicular tissue.
Does chemotherapy have an effect in the treatment of metastatic prostate cancer?
Chemotherapy in prostate cancer is the first choice in castration-resistant metastatic disease.
In 2015, CHARTED and STAMPEDE studies showed that there was an approximately 13-month prolongation in life expectancy with chemotherapy in the presence of a newly diagnosed hormone-sensitive but high-volume matastatic disease (visceral organ metastasis, 4 bone metastasis or extra-vertebral bone metastasis). Thereupon, the treatment algorithm in prostate cancer has changed and subsequent studies have shown that some androgen receptor blocker drugs (abiraterone, enzalutamis ..) increase the life span just like the chemotherapy (Docetaxel). Today, chemotherapy / immunotherapy is used in combination with “androgen deprivation therapy-ADT” (LHRH analogue / antagonist) in metastatic prostate cancer, regardless of low or high volume.
Does radiotherapy have an effect in the treatment of metastatic prostate cancer?
The results of the STAMPEDE study, published in 2018, showed that in patients with low-volume metastases (<4 bone metastases and no extravertebral metastases, no organ metastasis), radiotherapy to the prostate prolongs the life span. In these patients, radiotherapy for prostate and/or metastasis can be applied.
Does surgery have an effect in the treatment of metastatic prostate cancer?
There are studies showing the effectiveness of local treatments (Radical prostatectomy or radiotherapy) in metastatic prostate cancer.
Patients’ reservations about treatments
Incontinence
After radical prostatectomy, urinary incontinence is one of the most anxious issues for patients. The early urinary incontinence after surgery decreases over time with the strengthening of the auxiliary muscles. In the first year after surgery, the rate of complete dryness of patients is reported between 80% and 97% in different clinics. The age of the patient, the presence of urinary retention problems before the operation, the protection of the bladder neck during the procedure and the experience of the surgeon are important factors affecting postoperative urinary incontinence.
Erectile dysfunction
Another situation that can be seen after radical prostatectomy and causes anxiety in patients is the problem of erection. Erection problems at different levels can be seen in 70-75% of patients after surgery. Of course, the surgical technique (nerve-sparing approach) and the preoperative erection capacity of the patient significantly affect the postoperative erectile dysfunction rate.
Also after radiotherapy, nearly half of the patients can have erection problems.
After LHRH agonists or orchiectomy surgeries, the testosterone level decreases too much, resulting in erection problems and reducing libido.